NHN Resource Library
COVID-19 TELEHEALTH/TELEMEDICINE RESOURCE GUIDE
Current Public Health Emergency: Renewed Jan. 19, 2022
Quick Links
Update
- CMS List of Telehealth Services (as of 4/7/21)
- CMS MLN: Billing Telehealth Services correctly: as of 4/16/21. Watch the Medicare Coverage and Payment of Virtual Services video to help you bill correctly.
Recent Updates
- CMS COVID-19 FAQ’s (updated 03/31/2021 and includes Telehealth section-starting on page 66)
- CMS Telehealth toolkit: (Revision date March 2021)
- New Medicare Payment for COVID-19 vaccine administration: (effective 03/15/21)
- CMS MLN regarding Biden-Harris Administration Increase:(special edition - 03/15/21)
- FCC and COVID-19 Telehealth Program (Round 2 as of 03/31/2021): Rules and Guidance
- PHE Waiver updates: (02/19/2021)
- Provider Telehealth resources: (HHS.GOV)

What is Telehealth?
There are differences between Telecare, Telehealth, and Telemedicine. All three indicate that remote services are being provided from a health-care professional to a patient. However, the intent and technology differences of the services are defined below.
TELE CARE
TELECARE relates to technology that enables patients to maintain their independence as well as safety in their own homes. (Allowing patients to track their lifestyle changes over time)
- Examples: medical alert systems, a monitoring device
TELE HEALTH
TELEHEALTH is defined as remote-non-clinical services and audio-only.
- Examples: remote monitoring (Vital signs etc.), support staff health and patient education
TELE MEDICINE
TELEMEDICINE refers to remote clinical services completed by a provider/QHP and includes the use of both video and audio communication.
- Examples: Patient consultations-evaluation and management (E&M), remote/e-prescribe medications
Who Can Provide Telemedicine Visits?
- Physicians
- Qualified healthcare professionals (QHP), which includes:
- Nurse Practitioner (NP)
- Physician Assistant (PA)
- Nurse-midwives
- Clinical Psychologists (CP) and Clinical Social Worker (CSW) CPs and CSWs cannot bill Medicare for psychiatric diagnostic interview examinations with medical services or medical evaluation and management services. They cannot bill or get paid for Current Procedural Terminology (CPT) codes 90792, 90833, 90836 and 90838.
- Certified Nurse Mid-Wife (CNM)
- Certified Registered Nurse Anesthetist (CRNA)
- Clinical Nurse Specialist (CNS)
- Registered Dietitian (RD), or nutrition professional
- Therapists: Physical therapist, occupational therapists, speech-language pathologists, and psychologists can bill for e-visits using codes:
- G2010: Remote evaluation of recorded video and/ or images submitted by an established patient.
- G2012: Brief communication technology-based service (Virtual check in by a physician or other QHP who can report evaluation & management services provided to an established patient.)
- G2061: Qualified non-physician health-care professional online assessment and management service, for an established patient, for up to seven days, a cumulative time during the 7 days; 5-10 minutes.
- G2062: Qualified non-physician health-care professional online assessment and management service, for an established patient, for up to seven days, a cumulative time during the 7 days; 11-20 minutes.
- G2063: Qualified non-physician health-care professional online assessment and management service, for an established patient, for up to seven days, a cumulative time during the 7 days; 21 or more minutes
Tips for Excellent Documentation
- Use the same clinical guidelines you would with an in-person visit and bill accordingly based on thorough documentation.
- Set up a dedicated space for virtual visits
*And Document:
- If the visit was only audio or audio/visual
- What is the intent of the visit?
- What are the circumstances of the visit?
- Explanation of visit to patients-(non-face to face compared to in-office visit)
- Receive the patient’s verbal consent
- Most recent patient vitals with a note that states: vital signs will be taken at the next in-person/face-to-face visit
- Time spent on call
Most Common Tele-Billing Codes (per CMS)
| SERVICE | TIME | HCPCS/CPT CODES |
|---|---|---|
| Telehealth consultations, emergency department or initial inpatient | Varies | G0425-G0427 |
| Office or other outpatient visits | Varies | G0406-G0408 |
| Telehealth Pharmacological Management | Varies | G0459 |
| Individual psychotherapy | Varies | 90832-90838 |
| Medicare Annual Wellness Visit, includes a personalized prevention plan of service (PPPS) first visit | Varies | G0438 |
| Medicare Annual Wellness Visit, includes a personalized prevention plan of service (PPPS) subsequent visit | Varies | G0439 |
| Advance Care Planning | 30 min. | 99497 |
| Annual Depression Screening | 15 min. | G0444 |
| Psychotherapy for crisis | Varies | 90839, 90840 |
| Telehealth Consultation, Critical Care(patients/providers) initial visit | 60 min. | G0508 |
| Telehealth Consultation, Critical Care subsequent visit | 50 min. | G0509 |
Further review of CMS Telehealth services, (pages 7-10 coding guidance)
How Do I Bill for Telemedicine Visits and COVID-19
Place of Service (POS) Coding Guidelines
-
Per CMS: April 09, 2020
The IFC directs physicians and practitioners who bill for Medicare telehealth services to report the place of service (POS) code that would have been reported had the service been furnished in person. This will allow our systems to make appropriate payment for services furnished via Medicare telehealth which, if not for the PHE for the COVID-19 pandemic, would have been furnished in person, at the same rate they would have been paid if the services were furnished in person. We believe this interim change will maintain overall relativity under the PFS for similar services and eliminate potential financial deterrents to the clinically appropriate use of telehealth. During the PHE, the CPT telehealth modifier, modifier 95, should be applied to claim lines that describe services furnished via telehealth. Practitioners should continue to bill these services using the CMS1500/837P.
Example One
-
Patient John Doe has been receiving telehealth services since August 2019. The provider will continue to see John Doe via telehealth services through the Public Health Emergency (PHE). For the above service, bill POS 2; as telehealth service would have been used regardless of PHE.
Example Two
-
Patient Jane Doe is always seen in the clinic. As a result of the Public Health Emergency (PHE), the provider will now need to see her via telehealth. For the above service, bill POS 11; as telehealth services are new to Jane Doe as a result of the PHE as she would have otherwise been seen in the clinic.
Modifier Usage
As of June 1, 2020: Clarification for using the “CR” modifier and “DR” disaster and catastrophe related codes can be found here
Increased Tele-Visit Payments
Per CMS: April 30, 2020
CMS is broadening the list to include many behavioral health and patient education services. CMS is also increasing payments for these telephone visits to match payments for similar office and outpatient visits. This would increase payments for these services from a range of about $14-$41 to about $46-$110. The payments are retroactive to March 1, 2020.
CPT codes referenced: (Add 95 modifier and bill the same*Place of Service code you would have used if the service had been rendered in person)
- 99441 (5-10 minutes) $46.00
- 99442 (11-20 minutes) $75.00
- 99443 (21-30 minutes) $110.00
Recent Updates
- CMS COVID-19 revisions and update: (CR, DR and CS modifiers)
- CMS Medicare COVID-19 Vaccine Billing guide
- COVID-19 Treatment add on payments
- AMA 2021 E/M Revisions: bit.ly/38wn83D AND bit.ly/2MX0vgv
- Example: CPT code 99201 will be deleted as of January 1, 2021
- AAPC guidance
- Remote Patient Monitoring for COVID-19 (A telehealth delivery system - Mayo clinic): Remote Monitoring AND mayocl.in/38A3IuT
Definitions
- CR: This modifier is defined as “catastrophe/disaster related” and is used in relation to Part B items and services both institutional and non-institutional billing.
- DR: This condition code is defined as “disaster related” and used to identify claims that are or may be impacted by specific payer/health plan policies related to a national or regional disaster. The DR condition code is used for institutional billing only.
- CS: This modifier indicates that a member’s cost share should be waived for COVID-19 Testing. Use this modifier on visits only related to COVID-19 testing. (Can be used for both in person and telehealth visits)
- Telehealth Example: Billing a 99214 with both the CS, 95 modifiers (Since modifier CS affects payment, use this first)
Lab Billing
Per CMS: Jan. 25, 2021 publication
CMS updates lab payments for Iowa and Nebraska
| MAC JURISDICTION | MAC STATES/TERRITORIES | U001 TEST PRICE | U002 TEST PRICE | 87635 | 86769 | 86328 |
|---|---|---|---|---|---|---|
| J5-WPS | Iowa, Kansas, Missouri, Nebraska | $35.92 | $51.31 | $51.31 | $42.13 | $45.23 |
Lab Billing
Lab Continued
Related to COVID-19 testing on or after March 1, 2020:
- G2023 - Specimen collection for severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) (Coronavirus disease [COVID-19]), any specimen source
- G2024 - Specimen collection for severe acute respiratory syndrome coronavirus 2
- (SARSCoV-2) (Coronavirus disease [COVID-19]), from an individual in a skilled nursing facility or by a laboratory on behalf of a home health agency, any specimen source
New and Revised codes published April 10th and effective immediately:
- CPT 86318 (revision): Immunoassay for infectious agent antibody(ies), qualitative or semiquantitative, single-step method(eg, reagent strip)
- CPT 86328: severe acute respiratory syndrome corona virus2 (SARS-CoV-2), (Coronavirus disease - COVID-19)
- CPT 87635*: infectious agent detection by nucleic acid (DNA or RNA), severe acute respiratory syndrome-amplified probe technique. Corona virus2 (SARS-CoV-2), (Coronavirus disease-COVID-19)
- CPT 86769: Antibody; severe acute respiratory syndrome coronavirus 2 (SARS-Co-V-2)(Coronavirus disease - COVID-19)
*Antigen test code:
- CPT 87426: “Infectious agent antigen detection by immunoassay technique” used for testing of patients suspected of being infected with the novel coronavirus (SARS-CoV-2) bit.ly/3i37vUA
COVID-19 DIAGNOSTIC LABORATORY TEST
Billing for Clinician services Physicians and Non-Physician Practitioners (NPPs): Please see below CMS MLN link for related information regarding billing for COVID-19 symptom and exposure assessment and specimen collection performed on and after March 1, 2020: go.cms.gov/3sidkSL
- CMS Announces COVID-19 Antibody Treatment Access:
COVID-19 TESTING IN NURSING HOMES
PROCESSING OF ADD-ON CODES
Per May 15, 2020 MLN
There are several add-on services (CPT codes: 90785, 90833, 90836, 90838, 96160, 96161, 99354, 99355 and G0506), which Medicare may have denied during this PHE. MACs will reprocess those claims for dates of service on or after
March 1, 2020. go.cms.gov/3skrWRp
COVID-19 LOINC UPDATE PAGE
bit.ly/3oylXq1 and LOINC mapping for COVID bit.ly/3byiNin
CMS MLN UPDATES ON FQHC AND RHC FLEXIBILITIES
Additional guidance on telehealth services that have cost-sharing waived. go.cms.gov/2LGXr7J
TELEHEALTH'S IMPACT ON ACO ATTRIBUTION, per CMS
CMS clarified to NAACOS that all services listed in §425.400(c)(1)(iv) and, therefore, used in ACO assignment, will be counted in attribution when delivered via telehealth.
The CARES Act gave CMS broad authority to waive federal law and, in the March 30, interim final rule.
CMS:
- Activated six E/M CPT codes that are “telephone-only”
- CPT codes 98966-98968 and 99441-99443
- Added 80 additional CPT codes on the list for telehealth
- Relaxed restrictions on seeing new patients via telehealth
- Will allow face-to-face requirements to be filled via telehealth for hospice and inpatient rehab
- Will pay for services at “non-facility” rate
- Report the POS code as if the service been in-person. CMS finalized CPT telehealth modifier, modifier 95. Claims should not include the POS code “02-Telehealth” go.cms.gov/2Lu8wZM
AMERICAN MEDICAL ASSOCIATION GUIDELINES
Tele-Case Scenarios: Provided by the AMA
- Telehealth E/M-telephone assessment (Audio only- scenario 7)
- Telehealth for a non-COVID patient (Scenario 10)
- Telehealth for COVID concern not related to E&M and the patient is directed to come to the office or go to a specified location for testing. (Scenarios 3 and 4)
Example Scenario of COVID-19 CODING COLLECTIONS, TESTING AND DIAGNOSIS
Provided by Training Leader Health Care
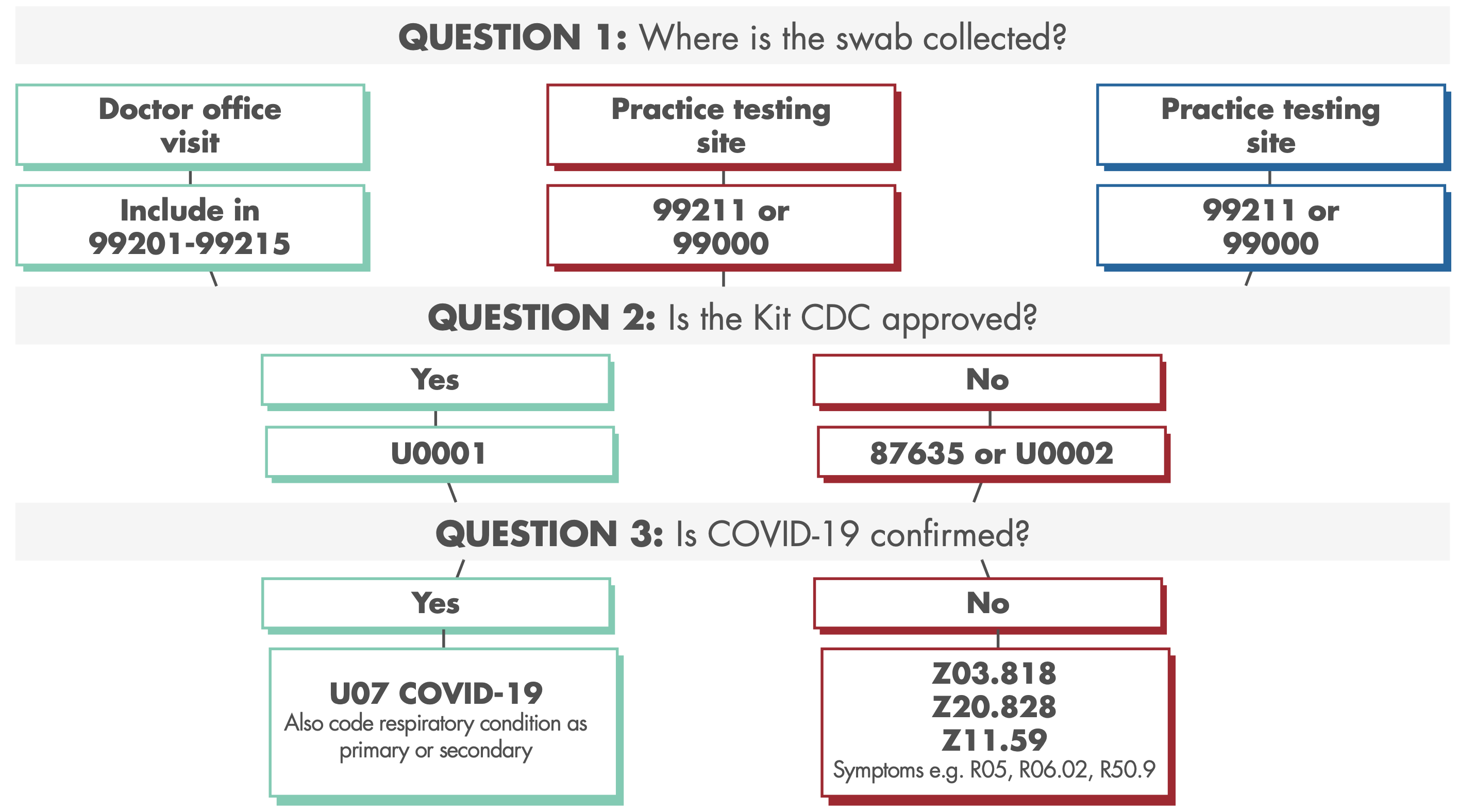
COVID-19 TESTING FLOWCHART
Pin Down Qualifying CPT and ICD-10 Codes
When a patient has a visit that results in testing for coronavirus, murky guidance makes it really hard to compliantly bill these services. Ask yourself three questions to identify the right mix of EM, lab and diagnoses that you should consider so you can accurately code your claim and capture every dollar you’re legally owed.
Additional Comments of the current Telehealth waiver: (may change when public health emergency(PHE) has been lifted)
Recent Updates
- AMA announcement of new COVID-19 vaccine CPT codes
- AMA - Find your COVID-19 Vaccine CPT Codes
- AMA-New code update for immunization (November 10,2020)
- American Medical Association adds two new multi-virus test codes (87636 & 87637)
- Vaccine-specific code update (AMA - November 10,2020)
- American Medical Association releases new CPT codes
- 86413 –This code was created to allow reporting of quantitative antibody detection of SARS- CoV-2.
- 99072 – Additional supplies, materials, and clinical staff time over and above those usually included in an office visit or other non-facility service(s), when performed during a public health emergency
Prescriptions
The Drug Enforcement Administration (DEA) has waived the need for face-to-face visits for controlled substances. DEA-registered practitioners may issue an electronic prescription for schedules II-V or they can call an emergency prescription for these into the pharmacy. The provider/prescription must meet the following conditions:
- The prescription is issued for a legitimate medical purpose by the provider acting within the scope of their practice.
- The communication is conducted using a platform that has audio and video capability, is in real-time, and is two-way interactive.
- The provider acts in accordance with federal and state laws.
HIPAA
Penalties for HIPAA violations with telecommunication platforms have been waived. Providers are expected to serve patients in good faith. Platforms such as FaceTime, Skype, WhatsApp, etc., are permitted during the public health emergency.
CMS-HHS.GOV: COVID-19 LESSONS LEARNED RESOURCE
bit.ly/39ucklZ and bit.ly/3ieOy1m
RECENT UPDATES
- DHHS COVID-19 info page: (tools and dashboards)
- Telehealth.HHS.GOV policy changes
- CMS COVID-19 TOOLKIT
- CARES ACT-2% Payment Adjustment
- CMS COVID-19 Updates (Webpage, Hotlines and Software)
CMS COVID-19 DATA REPORTING DURING PHE (CONDITIONS OF PARTICIPATION)
- Per CMS: COVID-19 laboratory test must be performed either during the hospital admission or prior to the hospital admission and must be demonstrated using only the results of viral testing (i.e., molecular or antigen), consistent with guidelines from the Centers for Disease Control and Prevention (CDC).
And CMS 20% add-on payment:
- Effective Sept. 1, 2020, the Centers for Medicare & Medicaid Services (CMS) has enlisted a mandate requiring hospitals to have positive COVID-19 laboratory tests in patients’ records to qualify for Medicare’s 20-percent add-on payment.
The 20-percent bonus applies to the DRG and does not affect patient liability, which continues to encompass the Part A inpatient deductible.
- MLN20015
- CMS COVID-19 Data Release: (External FAQ regarding the different data Medicare is sharing regarding COVID-19
- CMS updated COVID-19 FAQ as of August 26, 2020
RECENT UPDATES
- PHE extended (Through April 21, 2021):
- CMS PHE Extension Link (Telehealth)
- CMS Expansion of teleheath services (October 14, 2020):
- 11 new telehealth services go.cms.gov/3byhv79
- CMS COVID-19 Data Snapshot (November 30,2020)
- CMS PHE extension link (through January 21, 2021)
PAYER LINKS FOR TELEHEALTH AND COVID-19 GUIDANCE
- MSSP
- Additional CMS Telehealth service information
- CMS current emergency page
- For claims March 18, 2020, and through the end of the Public Health Emergency (PHE)