The CDC reports that people with higher patient activation, (the knowledge, skills and confidence to become actively engaged in their health care), have better health outcomes.
Patient activation exists far beyond the walls of our clinics. As health-care professionals, we need to ensure that we build trust at each health encounter.
Our communication, whether conducted during scheduling, within the clinical appointment, or through our follow-up materials; needs to guide patients and compel them to stay engaged.
According to the National Assessment of Adult Health Literacy, only 12% of U.S. adults have proficient health literacy skills. Health literacy is described as the degree to which individuals can find, understand and use information and services to inform health-related decisions and actions for themselves and others.
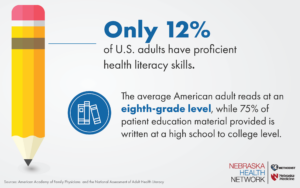
Many providers use educational resources, like the ones produced by the NHN, to support their conversations with patients. According to the American Academy of Family Physicians, the average American adult reads at an eighth-grade level. However, 75% of patient education material is written at a high school or above reading level.
When communicating with patients, keep the following tips in mind:
- Simple is best. Save the complex medical jargon for discussions with your peers. When communicating with patients, use simplified language that is easy to understand. For example, rather than describing a medication as “anti-inflammatory,” tell them it “stops swelling.”
- Avoid acronyms. Using unfamiliar acronyms and terms with patients creates a further divide between patients and their care teams. If acronyms are necessary or enhance the likelihood a patient will remember a concept, be sure to explain the meaning behind the acronym and include the full terminology in written communication.
- Meet the patient where they are. Consider language barriers and provide resources in multiple languages. Most of NHN’s patient resources are produced in English and Spanish. If you are in need of other languages, please let us know. Cultural competency training can help recognize differences and cultural preferences to help you build trust with patients with different backgrounds than your own.